Sharp doctor learns firsthand the importance of catching colorectal cancer early
As cases rise for people younger than 50, health experts call for recommended screenings to begin at age 45
Dr. Lee Remington-Boone vividly remembers the moment she got the news that would change her life. The Sharp Rees-Stealy family physician and her husband, Jeff Boone, had been waiting for the results of her colonoscopy.
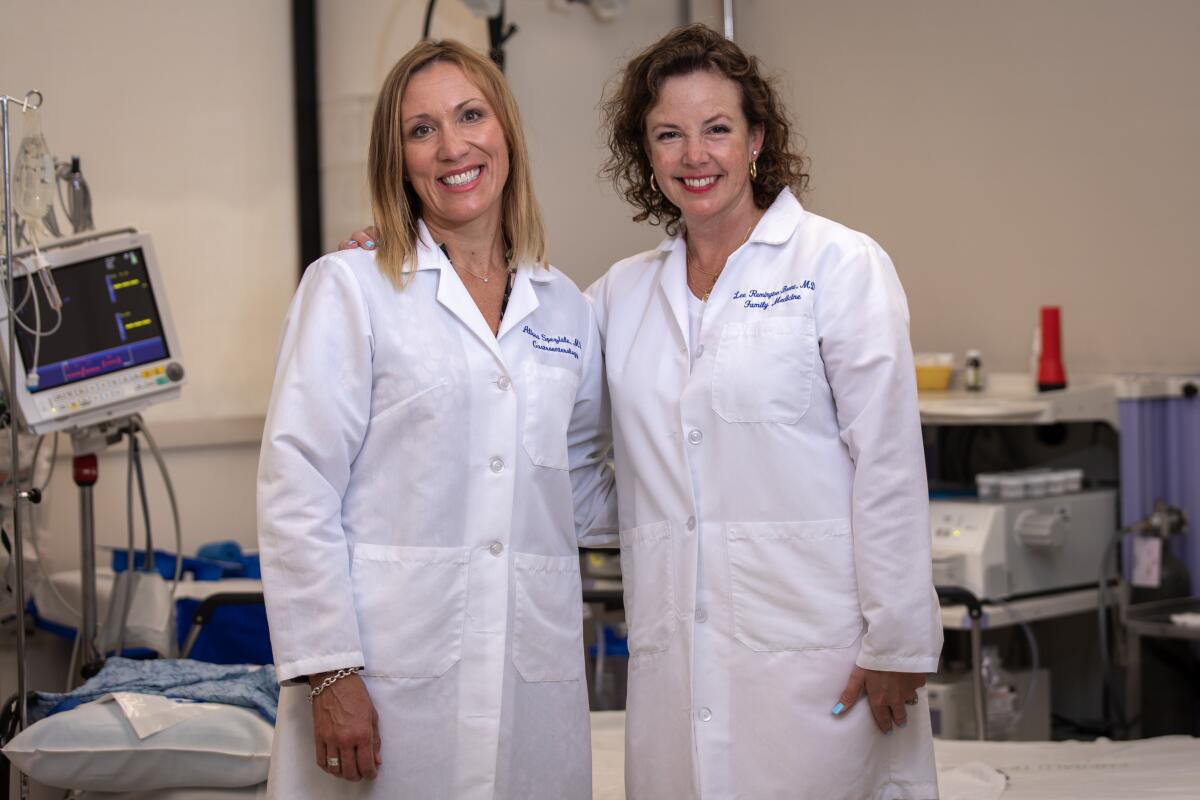
Sharp Rees-Stealy gastroenterologist Alissa Speziale told the couple that Remington-Boone’s screening indicated she had rectal cancer.
“We were devastated,” said Remington-Boone. “Anyone who’s gone through this remembers that — within the first hours of diagnosis — you don’t know what you’re facing. It’s overwhelming.”
She had no family history of colon or rectal cancer, nor was she in any high-risk categories for it. But at 48 — two years before screenings are currently recommended — Remington-Boone knew her body was signaling that something was wrong.
“Generally, I was a pretty healthy lady with a healthy diet. I wouldn’t call myself sedentary by any means,” she said. “I was going along doing my thing.
“Then I saw blood (in my feces), and thought: ‘What fresh hell is this’?”
Unfortunately, Remington-Boone is among the growing number of people under 50 who have been diagnosed with colorectal cancer. According to the American Cancer Society (ACS), colorectal cancer increased by 2 percent every year from 2012 through 2016 among people younger than 50.
ACS and other health organizations are advocating the government recommend colorectal screenings begin at 45 years old.
Many people were stunned by the news of actor Chadwick Boseman dying at the age of 43 from colon cancer last August. Best known for the groundbreaking film “Black Panther,” Boseman was actually in a high-risk group. The ACS reported that African Americans (whose recommended testing age is 45) are about 20 percent more likely to get colorectal cancer and about 40 percent more likely to die from it than most other groups.
But colorectal cancer affects many demographic populations.
The National Colorectal Cancer Roundtable, a health coalition that includes ACS and the Centers for Disease Control (CDC), said that an estimated 104,270 new cases of colon cancer and 45,230 cases of rectal cancer are expected to be diagnosed in 2021. It estimated 52,980 deaths from colorectal cancer are expected to occur.
Practicing gratitude
As a doctor, Remington-Boone knew that the ACS, CDC and other health organizations rank colorectal cancer as the third most common cancer and the second deadliest.
“I had a young patient in her late 30s who had rectal bleeding,” Remington-Boone recalled. “I kept saying she really needed to get a colonoscopy. She put it off until it was too advanced. She ended up dying at 42.”
After her own colonoscopy, Remington-Boone had to undergo a range of imaging procedures to determine the exact location of the tumor and how advanced her cancer was. She was terrified that her rectum might need to be removed.
The results were hopeful: Her cancer was Stage 1 and in an operable location.
Speziale, Remington-Boone’s gastroenterologist — and friend and colleague — said early detection of the cancer was key to the outcome.
“Lee had delayed for a while — doctors like taking care of others but not necessarily ourselves,” said Speziale, who is also Chief Wellness Officer at Sharp-Rees Stealy. “But we did check her out soon enough. Also, Lee had a very good partnership with her primary doctor who encouraged her and provided resources.
“That’s important — to be with a primary physician you’re comfortable with and feel confident about approaching uncomfortable subjects.”
Speziale added that Remington-Boone’s family provided invaluable support.
But early detection and a successful surgery doesn’t mean the ordeal is over. Yes, Remington-Boone is back to working regularly as a family physician and spends time with husband Jeff, son Connor, 21, and daughter Olivia, 18.
However, Remington-Boone is required to have colonoscopies twice a year for five years after her surgery. She has a yearly MRI of her abdomen and pelvis for indications of cancer spread.
“I revisit this in an intimate way every six months,” she said, adding that anxiety sets in about two weeks before each test. “It’s hard on my husband, especially the worry. He’s going through the milestones with me. Each passing interval, each subsequent test, it gets better.
“I have nothing to hook up. I’m not incontinent. Every day I practice gratitude. But there’s a chance of recurrence. My journey with it wasn’t as difficult as other cancer patients who go through chemo and radiation. But it’s impactful.”
The gold standard
Colonoscopies have a bad reputation. For most people, it’s not the sedation and procedure that gives colonoscopies a bad name. It’s the preparation. Adhering to a couple of days of strict diet and then consuming more than a gallon of clear liquid and laxative to cleanse the bowels is unpleasant. There are less bothersome alternatives, including at-home stool tests, which are covered by some insurance plans.
“The gold standard is the colonoscopy,” Speziale said. “Primary physicians encourage their patients to get them.
“The best part of a colonoscopy is not only that it provides a diagnosis, but it also removes pre-cancer polyps. Other testing strategies aren’t preventative.”
A colonoscopy helped save Remington-Boone’s life. A colleague told her that the pre-colonoscopy liquid tastes a lot better than chemo and radiation.
“The prep is the tough part,” Remington-Boone said. “But after that’s done, you get an awesome nap, get rid of any polyps, drop 6 pounds of water and you’re good.”
Symptoms of colorectal cancer
While acknowledging that more people under 50 are getting the disease, Sharp Rees-Stealy gastroenterologist Alissa Speziale noted she more commonly finds cancer among those over 50 who haven’t done their recommended screening.
“That’s heartbreaking,” Speziale said, “Because it means the cancer was preventable.”
One reason most doctors emphasize the importance of colonoscopies is that colon and rectal cancer don’t always cause symptoms until they’re quite advanced. That’s why it’s important to get a colonoscopy when your doctor says it’s time.
The following are some of the symptoms of colorectal cancer. They may indicate another medical problem, but your primary physician will know if a colonoscopy is needed.
- Rectal bleeding or blood in your feces
- A change in bowel habits — diarrhea, constipation or narrowed stools — that has continued for more than a week
- Persistent abdominal pain
- Weakness or fatigue
- Unexplained weight loss
“Cancers are metabolic and take a lot of energy,” Speziale said, explaining the last two symptoms. “It’s like having an alien in the body that’s sucking up all of its energy.”
That’s an excellent motive for getting colon screenings at the recommended intervals.
Sources: Alissa Speziale, M.D.; mayoclinic.org; cdc.gov; cancer.org; gi.org
Wood is a freelance writer.
Get Essential San Diego, weekday mornings
Get top headlines from the Union-Tribune in your inbox weekday mornings, including top news, local, sports, business, entertainment and opinion.
You may occasionally receive promotional content from the San Diego Union-Tribune.





